Head-to-Head: JCU should not have a COVID-19 vaccine requirement
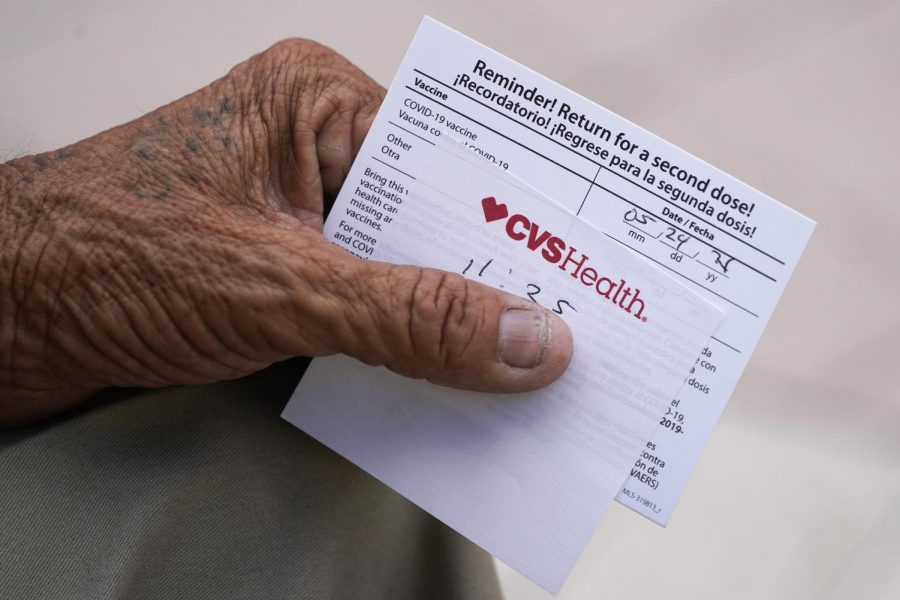
In this May 3, 2021 file photo, a man holds his vaccination reminder card after having received his first shot at a pop-up vaccination site.
Sep 27, 2021
Editor’s note: This opinion column is part of a faculty head-to-head series. Read the opposing perspective from Jim Lissemore and Medora W. Barnes, co-coordinators of the Program in Population and Public Health. Professors Frazier and Tarescavage have also submitted a letter outlining their recommendations for proceeding given the University’s decision to implement a vaccine requirement which can be found here.
“Follow the science” has sadly become a political buzzword, with the quiet modifier of if it supports your agenda never being said out loud. Although the natural and social sciences are objective (for the most part), the way some politicians, their appointed public health officials and other decision-makers use this information is not objective. Making things worse, large media corporations downplay and censor scientific information that does not fit with their preferred narrative. This puts individuals and societal leaders (who can be stuck in ideological echo chambers themselves) in a poor position to use all of the available research to more objectively inform their decisions. In part one of this column, we argue that the scientific literature supports making COVID-19 vaccines widely available. However, our comprehensive review of the research literature indicates that blanket vaccine mandates on college campuses are at best unnecessary, at worst harmful and in all cases unethical. Based upon our review of research, in part two of this column we make suggestions for how to move forward if vaccine mandates are continued at John Carroll.
To support our points, we list 23 scientific findings and other considerations. As you read through the list, we ask that you keep track of how frequently you have heard this information communicated by politicians, public health officials, or your preferred media sources. You may find that reading all of the scientific considerations (or at least a more comprehensive account than you had before) illuminates better ways to address the COVID-19 pandemic on college campuses.
Research Supports Making the Vaccine Widely Available
1. COVID-19 was the third leading cause of death in 2020, behind only heart disease and cancer. It is not yet clear how much COVID-19 contributed to these deaths, but the sheer numbers suggest that the contribution was substantial, particularly for older people and people with significant medical comorbidities.
2. The “original” COVID-19 strain was spread much easier than the flu.
3. The “delta variant” of COVID-19 is estimated to spread at a two times greater rate than the “original” COVID-19 strain.
4. As of this writing, Ohio hospitals are at 80% ICU bed capacity and 20% of ICU beds are occupied by COVID-19 patients. If COVID-19 infections and associated hospitalizations rise, care of all ICU patients (even those without COVID-19) would be negatively impacted.
5. COVID-19 vaccines decrease COVID-related hospitalization rates by about 30% (19 of 100 infected get hospitalized when not vaccinated versus 13 of 100 when vaccinated). Infection rates are also four to six times higher among the unvaccinated, which means that the large majority of COVID-related hospitalizations are among the unvaccinated.
6. COVID-19 vaccines decrease the spread of the “original variant” of COVID-19 by 40% to 50% to household members in “real world” experiments (i.e., not laboratory experiments that may not generalize to real-world settings).
7. The incidence of significant short-term side effects of COVID-19 vaccines are well under 1%. For people at risk of serious problems secondary to COVID-19, a simple cost-benefit analysis would indicate at this point that they are very likely to personally benefit from receiving the vaccine.
Summary: COVID-19 is a very serious public health risk. Vaccines are effective at decreasing this risk, both on a personal level by decreasing risk for serious COVID-related complications as well as on a community level by decreasing spread and hospital usage. The known risks associated with the vaccine are low, and at this point a simple cost-benefit analysis would indicate that getting the vaccine is probably a very good idea for many people.
Research Indicates that a Vaccine Mandate Should Not Be Used at College Campuses like JCU
8. The John Carroll University community was nearing herd immunity (if achievable) without a vaccine mandate. Herd immunity occurs when the percentage of people with immunity is high enough to effectively limit transmission of the infection. Based on an analysis presented in the medical journal Immunity, the herd immunity threshold for COVID-19 is approximately 67% – although it may be higher with introduction of the delta variant, as transmissibility is an important factor in herd immunity.
9. As of 8/27/2021, before the vaccine mandate was announced, the JCU COVID-19 dashboard reported vaccination rates of at least 59% among undergraduate students (66% of undergraduate students in residence halls). Faculty rates of vaccination were above 70%. Thus, based only on reported vaccine rates we were likely nearing herd immunity without a mandate (if herd immunity is even possible).
10. The number of JCU community members who have immunity to COVID-19 is higher than the number of people vaccinated because those who have had COVID-19 demonstrate immunity even if not vaccinated.
11. At least one in three Americans have had COVID-19.
12. Those who had COVID-19 have substantially greater immunity to COVID-19 than those who were vaccinated.
13. The vast majority of close contacts in a university setting will be among young and healthy people, who are at very low risk of serious complications from COVID. For example, there have been a total of approximately 3800 deaths from COVID among the over 125 million people under the age of 30. Put differently, only 1 in 36,000 young people have died of COVID-19, and the vast majority of deaths are individuals with significant underlying medical comorbidities.
14. Other methods can be used to substantially mitigate (and even eliminate) the risk of transmission at JCU to the most vulnerable (e.g., options for individuals to work and access resources remotely). The university is already equipped to enact these measures.
15. Vaccines will substantially reduce but not eliminate the possibility of a vulnerable person being infected and having serious complications as a result of COVID-19.
16. COVID-19 vaccines are associated with small but notable risks of side effects that are relevant considerations for younger people. For example, as concluded in a review of case studies published by the Journal of the American Medical Association, “Myocarditis may be a rare complication after COVID-19 vaccination in patients aged less than 19 years. In this case series study, the short-term clinical course was mild in most patients [who were hospitalized]; however, the long-term risks remain unknown. Risks and benefits of COVID-19 vaccination must be considered to guide recommendations for vaccination in this population.” Importantly, although some research would suggest that even for young people the risk of hospitalization secondary to COVID-19 is higher than the risk of hospitalization due to vaccine side effects, there are no focused studies comparing hospitalization rates for individuals who are both young and healthy. It may be that the risks of vaccination outweigh the benefits among young and healthy people, even in the short term. This is a reasonable consideration that has yet to be ruled out.
17. Close contacts with those who have asymptomatic infections from the “original” COVID-19 variant very rarely transmit disease according to an analysis of household spread of over 75,000 participants. Although spread from symptomatic individuals to household members occurred at a rate of 18%, asymptomatic individuals spread the virus to household members in less than 1 percent of cases. Even if one assumes that the Delta variant spreads at a two times greater rate, this would mean that asymptomatic spread would occur only 2% of the time in close contacts.
18. The FDA Approval of the Pfizer Vaccine indicated that the available information on the Pfizer vaccine “will not be sufficient to assess known serious risks of myocarditis and pericarditis and identify an unexpected serious risk of subclinical myocarditis.” For this reason, as a condition of approval, the company is required to conduct six additional studies to evaluate the occurrence of these medical risks over the course of 12/31/2022 through 5/31/2027.
19. The evidence that vaccination reduces community transmission in all relevant subsets of the population is weak. As noted earlier, there is only research supporting a 50% decrease in household transmission of the “original” COVID-19 variant across the general population of infected individuals who are vaccinated. However, there is no research to indicate a reduction in transmission with vaccination in young, healthy people or people with prior COVID-19 infection. Furthermore, any meaningful reduction in these groups is unlikely because younger adults are already at a 44% lower risk of contracting COVID-19 compared to individuals 20 years or older and far less than 1% of people who have natural immunity to COVID-19 are reinfected with the virus.
20. Approvals by US government health agencies are not necessarily healthy or ethical. Consider the infamous Tuskegee Syphilis Study, which was continuously approved until 1972 by the US Public Health Service (the institution that created the CDC). In this study, Black, Southern sharecroppers with syphilis were not offered penicillin by researchers when it became readily used to effectively treat the disease in 1943. Not only did many participants needlessly die, but several of their spouses were infected and they had children who were born with congenital defects as a result of the illness. Less than 50 years ago, a group of government-funded researchers saw no problem with this research. As asserted in a recent peer-reviewed article from the “British Medical Journal” on increased rates of vaccine hesitancy among individuals from Black populations, we agree that this finding is due in part to “previous unethical research in black populations.” We also agree that the solution is to “engage, listen with respect, communicate effectively, and offer practical support to those who have yet to make up their minds about the vaccine.” A blanket vaccine mandate runs counter to this solution.
21. There is emerging documentation showing that the National Institutes of Health (NIH) funded gain of function research in Wuhan, China in 2014. Less than 10 years ago, a group of government-funded researchers saw no problem with this research.
22. A lab-leak theory is now under serious consideration by the scientific community and government officials. Less than four months ago, lab-leak statements were censored on social media as misinformation. Things can change very fast in science and public health. We should be humbled by this and be very careful to judge things as unscientific or to label them as conspiracy theories.
23. The parasite-stress model of authoritarianism details how pathogens (e.g., infectious diseases like COVID-19) produce authoritarian behaviors that promote obedience at the cost of personal freedoms. Specifically, the incidence of pathogens in a country is very strongly related to the presence of authoritarian governments. Also, across 31 countries, the incidence of pathogens is very strongly correlated with authoritarian attitudes among individuals in that country. The reason for this association is thought to be that humans are hardwired through evolution to minimize risk of widespread death by pathogens at all costs, even if it causes substantial loss of civil liberties and even if this behavior is unnecessary given current scientific advances.
Summary: JCU has approached and potentially surpassed the bar needed to reach herd immunity (if this is possible), which indicates that there should be adequate immunity to limit substantial spread. Even 100% compliance with a vaccine mandate would not eliminate the risk of getting or transmitting COVID-19 at JCU. There are viable options that are not being used to eliminate the risk of transmission at JCU for the most vulnerable (e.g., remote work options). If young, healthy people are infected with COVID-19, they are at very low risk of serious problems, and they will have developed substantially greater immunity to the virus. Moreover, simple public health measures such as staying in one’s residence when experiencing symptoms will substantially limit transmission of COVID-19. Taken together, the obvious public health approach for JCU (which is not obvious until all the data is considered) involves common sense and freedom: give people the freedom to manage their own risks of contracting COVID-19 as well as the freedom to shelter themselves from this risk. This is in stark contrast to humankind’s hard-wired propensities for authoritarian behavior during pandemics, as predicted by the parasite-stress model.
It is necessary to establish that vaccination will reduce community transmission in all the relevant groups before a blanket mandate can be ethical (and other factors need to be established as well). At the present time, there is no evidence that vaccinating young, healthy people would reduce community transmission. In fact, the evidence suggests that vaccines are less likely to produce a meaningful reduction in community transmission in young, healthy people because they are naturally at a reduced risk of contracting COVID-19. Moreover, requiring vaccination for people with a history of COVID-19 infection (and thus have resulting natural immunity) is not supported by the available evidence. Instead, people with enhanced immunity due to prior infection may be exposing themselves to unnecessary risks associated with vaccines. Taken together, it is unethical to force a subset of the population (young, healthy people and those with natural immunity) to vaccinate if COVID-19 is not a significant risk to them, other readily-accepted risks are the same or higher (including daily risks such as driving – mortality is ~23 in 100,000 versus 10 in 100,000 for COVID-19 in ages 18-29), the vaccine’s side effects may pose greater risks than COVID-19, and there is insufficient evidence to demonstrate that vaccination reduces community transmission in these subgroups. There are also legitimate reasons for vaccination hesitancy (e.g., distrust in government institutions and the media). Ignoring those concerns and implementing a blanket mandate will likely increase vaccine hesitancy.
The long-term side effects of the vaccine are not known, which led the FDA to conditionally approve the Pfizer vaccine contingent upon the results of studies intended to investigate long-term side effects through 2027. Science is best understood as a process that takes time to produce reliable knowledge. Less than two years removed from the onset of COVID-19, and approximately nine months removed from the emergency use authorizations of vaccines, we are not in the stage of the scientific process where we can make authoritative statements that would lead to a blanket vaccine mandate.
Conclusion
Turning back to the question we raised at the beginning of this column, we ask that you reflect on how many of the 23 considerations that we presented are new and informative to you. If you feel so inclined, please indicate how many on this straw poll (you can also click to view the results).
Regardless of our agreements or disagreements on the issue of vaccine mandates, we suspect that many found at least one piece of new information to consider (not follow). This exercise illustrates how rigorous pursuit of the truth as a community, where all voices are heard, is the path forward. We hope that this article spurs more scientifically-informed decision-making at John Carroll University and beyond, and we hope that you will consider our solutions offered in part two of this column the path forward if vaccine mandates are retained.
Thomas Frazier is Professor of Psychology at John Carroll University. Anthony Tarescavage is Associate Professor of Psychology at John Carroll University.












Leslie Elia • Oct 2, 2021 at 11:05 pm
A few things were left out of this article, but it still makes me and my son stand our ground on not needing or wanting the vaccine for many personal reasons.
Thank you for writing the article and please continue to follow other sources of information other than mainstream news. I personally love the America Frontline Doctors, Dr.Robert Malone, Dr. Peter McCullough (cardiologist), Dr. Christiane Northrup (obstetrics and gyn), Dr. Martin Kulldorf (epidemiology), Judy Mikovits, PhD, Dr. Rashid Butter (osteopathy), Dr. Lee Merritt (orthopedist), Dr. Jim Meehan (ophthalmology and natural medicine), Dr. Carrie Madej (osteopathic medicine and bioscienses) and Dr. Jane Ruby.
A staff member • Sep 30, 2021 at 2:01 pm
You have failed to make your argument and go off on a number of irrelevant tangents logically. Sadly, personal “freedoms” have been weaponized by the far right (e.g., Jan 6, 2021 @Wash, DC), so in this case it is incumbant that the government “…provide for the common defense,[and] promote the general welfare…” of the whole population. You conflate free will with freedom. You demand ‘your rights’ but refuse to shoulder your responsibilities to others.
Rebecca Pettigrew • Sep 30, 2021 at 6:20 am
Excellent. Things you might add: 1) the vaccine is failing in countries and even US States which are highly. vaccinated. Cf. Great Britain and Israel and Vermont. 2) the vacccinated are still able to carry and spread the virus even whilst their internal system may enjoy protection (until they don’t, in which case it’s Booster time . . . again and again)
3) much of the data on hospitalization is skewed: if you are hospitalized for surgery or heart attack or car accident and are found to have CoVid (even if asymptomatic!) you are still considered a CoVid hospitalization. This significantly inflates our numbers on CoVid hospitalization. 4) we make policies as though there are no prophylactic practices or therapeutic treatments for CoVid, yet protocols have improved greatly since the onset of the pandemic. The virus can be deadly, yes, but early and vigorous treatment produces astoundingly better outcomes than what we saw in the very early stages in Italy, for instance. But media likes to keep the fear porn going and this administration and big pharm benefit financially from that irrational panic.
5) There are many countries who now admit the pandemic is over and that CoVid must now be considered endemic. We must learn to live with the virus and vaccination is one tool in the toolbox for those who don’t want to take the risk. For others, it is actually better to risk getting it and acquiring natural immunities which are broader and longer lasting.
6) it is entirely possible that by vaccinating even the healthy, young folks, we do the truly vulnerable grave harm as this accelerated the development of variants and their spread as the virus changes in order to get past the immune specific response triggered by the vaccine. Vaccinating only the at-risk population and making therapeutics widely and readily available would therefore be more just and equitable.
A professor • Sep 29, 2021 at 12:48 pm
It saddens me to see such a disingenuous and manipulative piece. Where to start? I will just pick on 3 things for now.
1. Two professors of psychology saying that human behavior accepting “authoritarian rule” can be “hard-wired”? Really? Even in birds the path from genotype to phenotype is a long and winding path. You know better than this.
2. Did we give up our civil liberties in the 1980’s when we agreed to seat belt laws? Did we give them up when we accepted getting 9 different vaccines growing up? Why are you wearing pants? How exactly is this vaccine the tipping point where we now accept the chains of our enslavement?
3. ” JCU has approached and potentially surpassed the bar needed to reach herd immunity (if this is possible).” Do you not see how contradictory this is? How can you possibly declare we’ve cleared the bar, when you simultaneously entertain that it might not even be possible? You know Delta is more transmissible. Obviously, the percent of vaccination to reach herd immunity is likely to be accordingly higher.
Dr. Tina M Facca-Miess • Sep 27, 2021 at 3:06 pm
This is a well researched, well written contribution to our community. For this I am deeply grateful. May God’s blessings follow.