Virus Models help Predict how the Return to Campus may have Looked
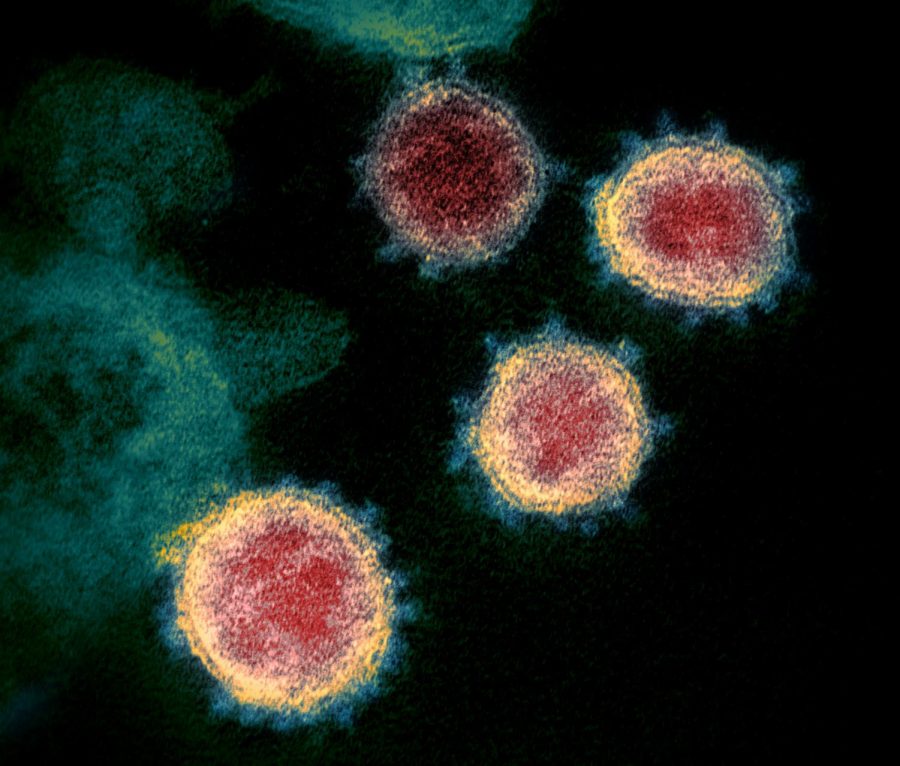
Photo from the Creative Commons
Microscopic cells of COVID-19 surround a group of healthy cells.
Sep 11, 2020
Biology professor Michael Martin asked what would happen if 10 John Carroll students were asymptomatic carriers of COVID-19, and the results were staggering.
An assessment published on the JAMA network (of the Journal of the American Medical Association) investigated what the COVID-19 case count might look like if college students returned to school. They found that just 10 asymptomatic students could cause a major outbreak.
Findings suggest that the only way to prevent this detrimental situation is to test every student every two days. The study concluded that testing symptomatic students wasn’t enough.
Martin asked if those conclusions would translate to John Carroll, and if so, what that would mean for the health of the John Carroll community.
Martin used the same viral reproductive numbers as the original study: 1.5, 2.5 and 3.5. The reproductive numbers measure how many people will be infected by one contagious individual. In other words, if the reproductive number is 1.5, every one person who is infected will spread the virus to another 1.5 people.
“In public health, we’re trying to get below one, which would indicate that the virus is not expanding,” Martin said.
“[The reproduction rate] is a moving target. The reproduction rate today would be different than what we might find a week from now, a month from now, in a different area of the country. … Things that keep the reproduction rate lower would be wearing masks, physical distancing.”
The variable of student movement and socialization is incorporated into the reproduction rate, but this variable is something universities have difficulty controlling.
“[The University of] Dayton, in my opinion, has a pretty bad problem at the moment,” said Martin. Though Dayton implemented COVID-19 precautions like physical distancing and masks, they have averaged 19 new cases per day in the last seven days and have a total case count of nearly 1,200. That’s almost 15% of their undergraduate population.
“The reason we are here … in this pandemic … is that the fraction of individuals that are going to be infected is in great part due to the number of individuals who are asymptomatic or pre-symptomatic. … Those people are able to spread the virus,” said Martin.
Young adults are at a lower risk of serious COVID-19 complications, but Martin says it isn’t that simple.
“This is not a two-outcome event. It’s not life or death. If it were simply life or death, we might view it in different ways. Those who live might have long-term or life-long chronic issues because of this. We see some evidence at the moment, but we’re still too close to when this thing started to have an understanding of what the longitudinal effects of this are going to be. That to me is a grave concern.
“Being 18-22 years old and then trying to manage a semester or a year in college where you leave your dorm room to go to the common bathroom, and you come back, and you’re out of breath … is a problem.”
In assessing what John Carroll would look like if students returned to in-person classes, Martin was not concerned about infection occurring in the classroom, but in the dorms. In John Carroll’s original HyFlex plan, students were to attend in-person classes for approximately half of the scheduled class meetings and then receive online instruction for those remaining. For the HyFlex approach to work, students were invited back to the residence halls. Though professors can ensure masks are worn and a six-foot distance is maintained in the classroom, students are responsible for their own safety once class ends, which caused major concerns for both Martin and the administration.
“If Notre Dame and Dayton are examined as models, perhaps [a reproduction rate of] 3.5 is not enough. You can imagine how living in a dorm or in a house off campus means it’s very difficult to distance yourself from each other. The virus can tear through communities that way.”
The factors of living arrangements, hand washing, wearing masks and congregating in large groups greatly affect the spread of the virus. Living arrangements are a major concern in controlling an outbreak.
“I have some pretty big concerns about a party in a front yard on Warrensville Center Road. It’s not good. It doesn’t look good in the community. People drive by and think about college students and what they might be doing. When it gets colder and that party moves into the basement of the house, it will get much worse.”
“[The need for socialization] might be greater than usual, and that’s going to act against being able to prevent outbreaks. … It’s a sacrifice, there’s no doubt about it. … I’ve seen my mother twice since Christmas. I don’t want to deliver this thing to her. I don’t want to think about how I killed my mother. What a terrible thing to think about.”
Martin sent his model to the administration before the transition to online courses was announced. John Carroll has now transitioned to solely online instruction for the remainder of the fall semester.
“[Students must realize that] activating this virus in our community has consequences to our students but also to the community of faculty, staff and employees at the university, and the areas around us as well.”
Martin concluded by saying, “I’d think Dayton, if they could go back in time, would remake that decision. It’s certainly harder to have a population that’s living in fear and anxiety of getting sick than it would be to have them come at a later date.”